| TH E N I H C A T A L Y S T | S E P T E M B E R – O C T O B E R 2008 |
| | |
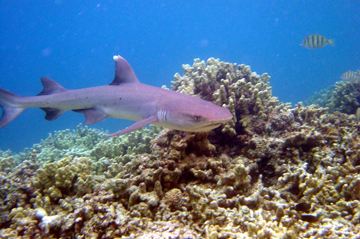
Back in the early 1990s, the shark cartilage craze was in full bloom. Inspired by a best-selling 1992 book "Sharks Don't Get Cancer," both healthy people and those stricken with cancer were popping pills of pulverized shark cartilage with hopes of staying healthy or even completely curing themselves of malignant tumors.
The logic, according to author William Lane, was that sharks rarely get cancer compared with most other animals, and the defining feature of their biology, aside from a healthy diet of fish, was a skeletal system made of cartilage rather than bone.
Mass hysteria ensued as holistic enthusiasts sought over-the-counter quick preventatives at the expense of the shark population. Unfortunately, shark cartilage did not live up to its reputation. Contrary to the book's bold title, sharks do sometimes get cancer. Up to 42 different types of cancer have been documented so far, including cartilage cancer.
Yet all animal cartilage does have anticancer properties. While the use of cartilage as medicine has not yet proven fruitful, NIH intramural scientists have identified unique characteristics in cartilage that someday could be exploited to slow or stop cancer growth. The research hopes to bring out the shark in all of us.
From the Ashes of Clinical Trials
Researchers have known for decades that cartilage has therapeutic properties. Studies from the late 1960s revealed that bovine cartilage reduced inflammation. Building on this, research from the 1970s found that bovine cartilage contains a substance that blocks angiogenesis and thus could check tumor growth.
The 1980s brought laboratory and animal studies and the first clinical trials testing bovine cartilage as a treatment for cancer. Gradually the research turned to shark cartilage, because pound for pound, sharks have more cartilage than cows. Also, researchers thought that shark cartilage might be more active than bovine cartilage in preventing new blood vessels from being formed.
To date over a dozen clinical trials have been conducted on shark cartilage as a cancer treatment. Seven of these studies have been published. Even though preliminary experiments in cell culture showed reduced cancer cell growth, none of the trials have yielded positive results.
The most recent clinical trials, sponsored by the NCI and the Mayo Clinic, involved a liquid extract of shark cartilage called Neovastat, administered orally. These, too, failed to produce positive results in cancer patients and have since been halted.
But the research isn't dead. Research at NIH demonstrates how following up on the anticancer properties found in cartilage or other tissues has led to new types of therapeutics. Labs are focusing on identifying specific candidates in tissues, rather than using whole slurries of dead animals, and they are showing much more promising results.
Enter the Matrix
Cartilage is composed of sparsely distributed chondrocytes and an extracellular matrix (ECM). The ECM is a web of structural proteins—such as fibronectins, collagens, laminins and proteoglycans—that provides a scaffold that holds the tissue together. Because this tissue needs to be mechanically strong, there are fewer cells and blood vessels than in other tissues.
Cartilage's unique and imposing structure makes it nearly immune to cancer growth. It is difficult for cells to penetrate through the network of ECM, thus thwarting metastasis.
"Sharks may be less likely to get cancer than humans because of their abundance of ECM, which just so happens to be a major component of cartilage," said David Hall, group leader of the NIAMS Cartilage Biology and Orthopaedics Branch, who had studied the cartilage-anticancer connection for several years before turning more of his attention to osteoporosis and arthritis.
For cancerous cells to thrive and spread, they need an abundance of nutrients to aid in growth and ways to escape to new tissues. Many cancers secrete high levels of matrix metalloproteases, or MMPs, which essentially chop up the ECM, allowing the cancer cells unhindered movement to invade other tissues. Cancers also secrete angiogenesis factors to create new blood vessels so that nutrients and oxygen can be brought to the tumor.
Cartilage and the ECM have protection mechanisms in place to ensure that their environments limit the movement of invading cells, MMP activity and blood vessels formation. In addition to its structural components, ECM contains regulatory proteins that control how cells behave.
"It's the normal ECM that is a physical and biochemical barrier that has to be overcome in order for metastasis to occur," said William Stetler-Stevenson, a senior investigator in NCI's Cell and Cancer Biology Branch. "There are components of the ECM that function to suppress the process and the events associated with growth, invasion and metastasis."
Stetler-Stevenson's group's studies of the anticancer properties of ECM have lead to promising new therapies and may reveal the initial anticancer effects that were observed using shark cartilage in cell-culture studies.
There Will be Blood, Or Not
David Roberts, head of the Biochemical Pathology Section in NCI's Laboratory of Pathology, has focused on two angiogenesis-inhibiting thrombospondin proteins that are released in the ECM, TSP1 and TSP2. These proteins bind to the components of the ECM and activate receptors that tell the cell not to grow or migrate. In many cancers found in animals and humans, levels are thrombospondin are reduced, which allows new blood vessels to form and deliver a supply of fresh nutrients to the tumor.
Therapeutics have been designed to block the angiogenesis pathway based on research from Roberts' lab and others. Although they have been proven somewhat effective, they are flawed. "They extend life by several months, but there is a problem because these patients get hypertension," he said.
Roberts' lab has shown that TSP1 is a potent antagonist to nitric oxide. The lab first observed that TSP1 was 100 times less effective in cell culture assays than it was when circulating in the bloodstream. They discovered if they added back nitric oxide to the cells, TSP1 increased in potency.
It is through inhibition of nitric oxide signaling that TSP1 is responsible for preventing angiogenesis. But "nitric oxide wears different hats in the vascular system," Roberts said. Nitric oxide is responsible, for example, for normal homeostasis of blood vessels by causing them to relax. When nitric oxide signaling is repressed, the blood vessels contract, which leads to high blood pressure.
Roberts' research has undoubtedly demonstrated that specific angiogenesis inhibitors will have to be selected more carefully to not interfere with blood pressure homeostasis.
 |
 |
 |
The Matrix: Reloaded
Stetler-Stevenson works on a very different ECM protein that is a major soluble component of cartilage, called TIMP2, for tissue inhibitor of metalloproteases. As the name suggests, TIMP2 can bind and directly inhibit MMPs. MMPs are responsible for inducing cell proliferation in response to growth factors, signaling proteins that promote cell growth. Adding TIMP2 to cells inhibits MMPs, causing a reduction in growth even in the presence of growth factors.
As a result of the TIMP experiments, MMP inhibitors seemed like a great potential cancer therapy. "Drug companies invested hundreds of millions in MMP inhibitors that worked great in mouse models but had no effect in human cancers," said Stetler-Stevenson. Naively, it was not realized that MMPs are both positive and negative enhancers of growth and migration.
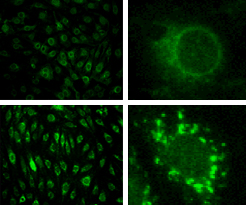
Stetler-Stevenson's lab created a version of TIMP2 with an extra alanine at the beginning of the protein that prevented TIMP2 from binding and inhibiting the MMPs. Surprisingly enough, this variation of TIMP2 was still able to prevent cell growth, demonstrating that TIMP2 had a function aside from MMP inhibitor. The lab soon determined that TIMP2 also binds to a cell receptor known as α3β1 integrin, which sends signals to inhibit growth responses. This integrin response regulates normal homeostasis in the cartilage.
"Tumor cells make such a large and diverse spectrum of MMPs that acts as a sink, and the TIMP gets bound to all those and there is none left to act with the α3β1 integrin," Stetler-Stevenson said. His group injected a small protein version of the TIMP2 with the extra alanine into tumors, which did not bind the MMPs, but bound α3β1 integrin. The integrin then sent signals telling the tumors to not grow or migrate. These studies have been done successfully in cell culture and now the lab is moving on to mouse models.
"[TIMP2] is a good potential cancer therapeutic because it's an endogenous protein, and we're trying to use what the body already makes," Stetler-Stevenson said.
"People used to think that matrix proteins were just the glue that holds cells together," said Roberts. Sharks may have clued us in that there is something special about cartilage, and by focusing on cartilage and ECM biology, we may find cancer therapeutics right in our own bodies.