|
Francis
Collins,
director, NHGRI (at NIH since 1993): What’s next after you’ve
mapped the human genome?—a human haplotype map to chart the variants
that contribute to common diseases–an international project involving
six countries and support from 18 NIH institutes
|
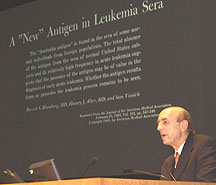 |
Harvey
Alter,
chief, CC Infectious Diseases Section (at NIH since 1969); Co-discoverer
of the Australia antigen, eradicator of posttransfusion hepatitis, and
poet: "When I came to NIH as a lowly fellow, I saw that patients
were turning yellow . . ."
|
 |
Elizabeth
Neufeld, professor and chairman, biological chemistry, UCLA David
Geffen School of Medicine (at NIH 1963–1984)) devoted to the study
of lysosomal enzyme deficiencies, recalled the "inadvertent mix in
the Petri dish of Hurler and Hunter cells, which together produced a normal
pattern—proving that two wrongs can make a right"
|
 |
Tony
Fauci, NIAID director (at NIH since 1968): Seeing AIDS patients
for the first time on the CC’s 11th floor, "I didn’t fully
appreciate this was a new disease, but I was anxious because I couldn’t
understand it. . . . I turned over my (host immune defense) lab to the
study of HIV"
|
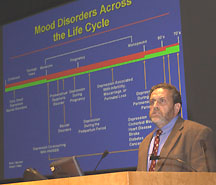 |
Dennis
Charney, chief, Mood and Anxiety Disorders Research Program, NIMH
(at NIH since 2000): Collaborative proof-of-concept trials are underway
that aim at new targets to fight depression, an underappreciated, crippling
disorder that can potentiate conditions like heart disease, diabetes,
and osteoporosis
|
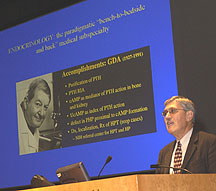 |
Allen
Spiegel, NIDDK director (at NIH since 1973), world-renowned for
his research in G-protein dynamics and hormone disorders, paid homage
to his NIH mentor G.D. Aurbach, who purified parathyroid hormone and launched
the study of signal transduction disorders
|
 |
Henry
McFarland, director, Clinical Neurosciences Program, NINDS (at
NIH since 1976): "[Early on], multiple sclerosis is inflammatory;
later it’s degenerative. . . . There are both upregulated and downregulated
genes. . . . The key is to conduct small trials of innovative therapies"
|
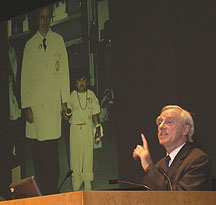 |
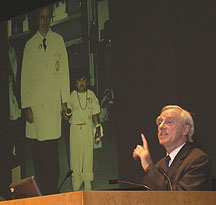
French
Anderson, director, Gene Therapy Laboratories, USC Keck School of
Medicine (at NIH 1965–1992), shown with the first gene therapy patient—age
4 in 1990—whose adenosine deaminase levels are still normal. He asks:
"Why is it that she has been able to develop a T-cell response to
new antigens? Did some stem cells get in there? Can T cells de-differentiate
and be reeducated?"
|
 |
 |
|
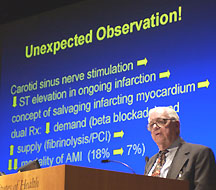
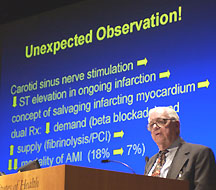
Eugene
Braunwald,
Hersey distinguished professor of medicine, Harvard Medical School (NIH:
1955–1968; hangout: CC, 7th floor, cardiovascular physiology lab):
Thanks to the disobedience of a patient on self-activated carotid sinus
nerve stimulation, it was learned that ST segment elevation decreases
in the midst of an ongoing infarct—and the concept of myocardial
salvage was born. With b-blockade and fibrinolysis,
acute MI mortality dropped from 18 to 7 percent
|
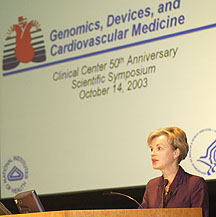
Elizabeth
Nabel, scientific
director for clinical research, NHLBI (at NIH since 1999): Genomics and
stem cells are involved in much of cardiovascular disease research at
the CC today. Researchers are correlating gene polymorphisms with drug
sensitivity and with the propensity for restenosis, and injecting endothelial
progenitor cells into ischemic scar tissue to repair vascular damage
|
| |
|
 |
Vincent
DeVita,
professor of medicine, epidemiology, and public health, Yale University
(at NIH 1963–1988, as NCI director from 1980): Lead author of the
1970 Annals
of Internal Medicine report establishing that some advanced cancers
could be cured by combination chemotherapy, a strategy that launched the
era of cancer survival, with rates going from 0 to 80 percent today for
some cancers
|
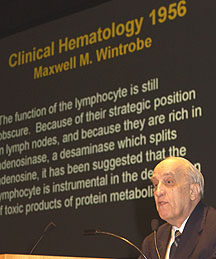 |
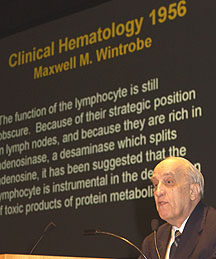
Thomas
Waldmann,
chief, Metabolism Branch, NCI (at NIH since 1956, when, according to the
textbook in the background, "the function of the lymphocyte [was]
still obscure"): Developer of anti-TAC, the first antibody to a cytokine
receptor (IL-2Ra)—used clinically in the
management of cancer, transplant rejection, and autoimmune disease and
in studies underway at six NIH institutes. The IL-2/IL-15 interface now
commands much of his attention. The T cell, Waldmann says, "is the
sun of the immunological system"
|
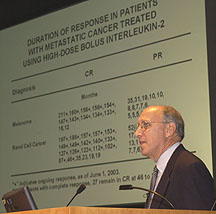 |
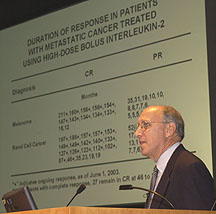
Steven
Rosenberg, chief, Surgery
Branch, NCI (at NIH at this post since 1974): A 30-year odyssey to develop
cancer immunotherapy has established that this approach can achieve cures;
tumor-infiltrating lymphocytes and tumor-specific antigens are central
to a strategy whose latest development involves nonmyeloablative conditioning
followed by adoptive transfer of antitumor lymphocytes targeting specific
tumor antigens
|