| T H E N I H C A T A L Y S T | N O V E M B E R – D E C E M B E R 2002 |
|
|
|
Menopausal Hormone RxDISPARATE VOICES REFLECT ON WHI DATA,ICS LOOK TO FUTURE |
by Fran Pollner |
"The reaction to a new scientific finding is proportional to the strength of the dogma it overturns."
—Elias Zerhouni, concluding the scientific workshop on menopausal hormone therapy, October 24, 2002
|
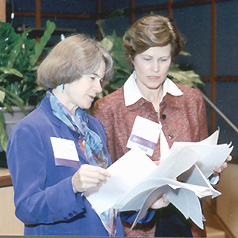
NIH
Deputy Director Ruth
Kirschstein (left) welcomes former NIH director Bernadine Healy, who
launched the Women’s Health Initiative in 1991; behind them is NIH
Director Elias Zerhouni
|
When the Women’s Health Initiative (WHI) halted the estrogen-progestin arm of its hormone study last July, a bit of medical dogma bit the dust. That dogma held that hormone therapy protects postmenopausal women against heart disease; the part overturned related to the hormone combination most prescribed in this country for postmenopausal women with an intact uterus.
The ensuing strong reactions found a forum for expression at a scientific workshop here October 23–24 to review those WHI results and their implications for clinical practice and future research.
NIH took some heat for the way it had handled the halting of the studyand the way it had notified the public and the medical community of the unexpected findings—criticisms NIH Director Elias Zerhouni said NIH had taken to heart. Women’s health advocates also decried the fact that promotional claims for the regimen under study had overstepped scientific evidence, unduly influencing the choices of women and their doctors.
The predominant concerns voiced during the workshop, however, were that the results not be extrapolated to all hormone formulations and doses and that research proceed on the risks and benefits of these and other treatments for individual women seeking relief from acute menopausal symptoms—as well as for prevention of the chronic conditions the WHI is designed to study: heart disease, osteoporosis, and breast and colorectal cancer. Many emphasized the need for fundamental research on hormonal signaling systems.
Background
Last July, NHLBI, in agreement with the Data Safety and Monitoring Board (DSMB) of the WHI halted the combination estrogen-progestin arm of the WHI hormone study three years before its scheduled conclusion. (For an extensive index on the WHI and related material on postmenopausal hormone therapy, see this website.) Not only did the postmenopausal hormone regimen not confer cardiovascular benefit—an expected beneficial outcome that the study was designed to quantify—but women on active drug actually had a higher rate of heart attack and stroke than those on placebo. They also experienced more thromboembolic events and breast cancer. Lower rates of osteoporotic fractures and colorectal cancer did not overcome the unfavorable risk:benefit ratio.
 |
 |
 |
|
Vivian
Pinn, director, Office of Research on Women’s Health (ORWH)
emphasized the need for evidence-based practice: "The bottom line
is that we now have more information for women to make informed decisions."
Pinn co-chairs the WHI with NHLBI Director Claude
Lenfant. The WHI is sponsored by NHLBI in cooperation with NIA, NIAMS,
and NCI. For background information on the WHI, see the website
and the WHI participant website (with
access to the videocast of the scientific worshop)
|
WHI
principal investigators Marcia Stefanick (left) and Marian Limacher, professor
of medicine and director of preventive cardiology, University of Florida,
Gainesville, presented data that "removes combination hormonal therapy
from coronary heart disease prevention strategy" for both primary
and secondary disease and across the WHI age spectrum of 50–79. Major
medical organizations and the clinic/ issued statements in agreement.
|
WHI biostatistician Garnet Anderson, Fred Hutchinson Cancer Research Center, Seattle, fielded charges of WHI "selective detection bias" in the breast cancer findings, noting that regardless of whether some women knew what they were taking, the mammography rates in both the active-drug and placebo groups were "exactly the same and the outcomes were completely blinded. It was as rigorous as a clinical trial could be for women with a uterus." |
 |
||
|
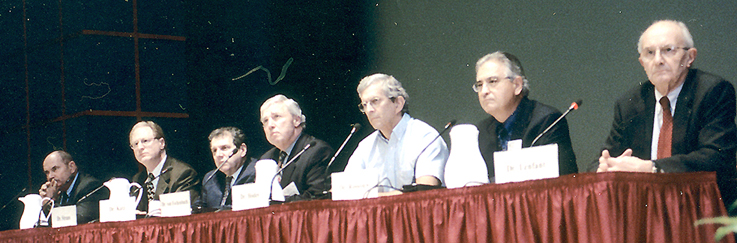
Outlining
their extensive ongoing and projected basic and clinical research agendas
on the effects of hormones and other agents on menopausal symptoms and
postmenopausal aftereffects were NIH directors (left to right) Duane
Alexander, NICHD; Steve
Straus, NCCAM; Stephen
Katz, NIAMS; Andrew
von Eschenbach, NCI; Richard
Hodes, NIA; Jacques
Rossouw, acting director, WHI, NHLBI; and Claude
Lenfant, NHLBI
|
||
The cardiovascular risks emerged early in the study, persisted, and were sustained in all age groups (of the 16,600 women enrolled in the trial, 30 percent were 50–59, 45 percent were 60–69, and 25 percent were 70–79).
The findings were especially jarring because they flew in the face of observational studies and the climate of acceptance that had informed the prescribing habits of many clinicians with menopausal and postmenopausal patients. When the study was halted and results made public, millions of women and their physicians were left in a quandary.
The investigators themselves had been "shocked" on two even earlier occasions when the DSMB told them to inform study participants, first, that a small increase in heart attack, stroke, and blood clots in the legs and lungs had been identified in the combined-hormone cohort and, later, that the risk had not disappeared with time, recounted WHI steering committee chair, Marcia Stefanick, of the Stanford University Center for Research in Disease Prevention.
Torrents of Data To Come
A tremendous amount of data is yet to come from the WHI—from the halted study as well as from the continuing trials involving unopposed estrogen in hysterectomized women, dietary modifications, calcium and vitamin D, and overlapping regimens, which are scheduled to continue for several more years.
A priority of WHI investigators
is to start publishing additional findings from the estrogen-progestin trial
within six months. They plan to examine correlations of genetic, biochemical,
and coagulation biomarkers with outcomes to identify subgroups at greater risk.
They will also study whether regimen-related harms dissipate over time after
discontinuation. Additional publications will address cognitive function—also
the subject of a WHI ancillary study—and quality of life, as well as underlying
differences among the women in the estrogen-only and combination cohorts. ![]()