| T
H E N I H C A T A L
Y S T |
J A N U A R Y - F
E B R U A R Y 2000 |
|
GENE
THERAPY TRIAL
AND ERRORS
RAISE SCIENTIFIC,
ETHICAL, AND OVERSIGHT
QUESTIONS
|
by
Fran Pollner |
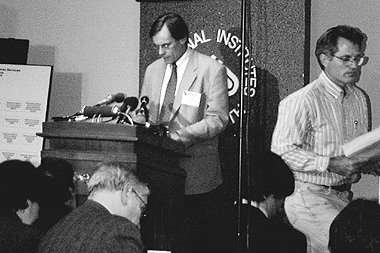
University
of Pennsylvania gene therapy researcher James Wilson reads a prepared statement
at a press briefing after the first day of the RAC proceedings in December.
The RAC meeting was convened to review the track record of adenoviral gene
therapy vectors and the conduct of the UPenn protocol that resulted in the
death of patient Jesse Gelsinger. Wilson was introduced by Paul Gelsinger
(right), Jesse Gelsinger’s father, shown exiting after delivering his
own statement and answering reporters’ questions. Wilson declined to
entertain questions.
Current
Event
Nearly
a decade after it permitted NIH intramural researchers to pioneer this country’s
first two human gene therapy trials—and some 350 diverse human gene therapy
protocols later—the NIH
Recombinant DNA Advisory Committee (RAC) held
a three-day assembly centered on the first reported death of a gene therapy
research patient attributed to the therapy itself.
The death last September
of Jesse Gelsinger, an 18-year-old patient with partial ornithine transcarbamylase
(OTC) deficiency, injected a sobering pause in a field rushing toward the 21st
century’s promise of an avalanche of gene therapy applications inspired
by the completion of the Human Genome Project and related discoveries.
The death also precipitated
an FDA freeze on the clinical trial in which Gelsinger was enrolled—a safety
and biological efficacy study of the recombinant adenoviral vector—OTC
gene delivered to the liver via the intrahepatic artery. Gelsinger was the scheduled
penultimate patient in what was to have been an 18-patient study and the second
one to receive the highest protocol-defined dose in this dose-escalation trial
that was begun in 1997 at the University of Pennsylvania in Philadelphia.
The pivotal speakers at
the RAC proceeding, held December 8 through 10, 1999, on the NIH campus and
under bright media lights, were the OTC study investigators: veteran gene therapy
researcher James Wilson, director of the Institute for Human Gene Therapy, and
surgeon Steven Raper, both of UPenn, and pediatrician Mark Batshaw, chief academic
officer at the Children’s National Medical Center in Washington. All three
apologized for communication gaps with oversight agencies and lapses in complying
with adverse event reporting requirements, which, had they been adhered to,
might have led to a protocol modification or a reevaluation of Gelsinger’s
candidacy for trial participation. Gelsinger’s precipitous and ultimately
irreversible response to the experimental therapy included signs of disseminated
intravascular coagulation (DIC), massive cytokine release, adult respiratory
distress syndrome (ARDS), and multiple organ failure.
The purpose of the meeting,
federal officials and RAC officers emphasized, was largely educational: to pool
information on the biology and toxicity of adenoviral vectors; to scrutinize
the conduct of the OTC trial with a view toward identifying red flags and improving
gene therapy trial design in general; and to revisit federal reporting requirements,
interagency communications, and the role of the RAC in gene therapy oversight.
Patient advocates, however, voiced worries that gene therapy research might
be stopped or curtailed; industry representatives cautioned against increased
public scrutiny that might bare trade secrets or misleading information; and
reporters wanted to know the specifics of protocol violations and any other
problems in the OTC study, as well as steps planned by overseers to enforce
compliance with scientific and ethical guidelines in the conduct of human gene
therapy research.
RAC chair Claudia Mickelson,
a bio-safety officer at the Massachusetts Institute of Technology in Cambridge,
and molecular biologist and former RAC chair Inder Verma, of the Salk Institute
for Biological Studies Laboratory of Genetics in San Diego, served as moderators.
Adenoviral
Vector Experience
According to Amy
Patterson, director of the NIH
Office of Biotechnology Activities (OBA, formerly the Office of Recombinant
DNA Activities), about 4,000 patients have participated in about 350 gene therapy
trials in the past decade; adenoviral vectors have been used in about one-quarter.
Immediately after OTC investigators notified OBA of Gelsinger’s death,
Patterson said, OBA notified the more than 70 other researchers currently using
similar methods in their own gene transfer studies.
After Gelsinger’s
death, the FDA conducted a database search of all gene therapy protocols with
adenovirus vector and found no similar ARDS, aplastic anemia, or extensive DIC
findings, an FDA official said.
A refresher course in
adenovirus basics was presented by experts summoned to the RAC proceedings.
Among the relevant facts noted were that adenovirus can cause fatal hepatitis
in immunocompromised individuals; and that adenovirus attaches to the coxsackie-adenovirus
receptor (CAR) in the liver, a receptor whose function and level of expression
in different tissues are not well known and whose abundance in the liver varies
among humans and animal models. To render adenovirus suitable as a gene vector,
viral genes required for replication are deleted; thus enfeebled, adenovirus
generally serves well as a vector. There are, however, some concerns regarding
viral infection: In simian species, adenoviral replication is enhanced in the
context of co-infection with another virus, such as SV40; and adenovirus can
also function as a helper virus, for instance, potentiating the growth of parvovirus.
Still to be understood is the ability of certain integrins that facilitate adenoviral
integration into target cells to induce cytotoxic and apoptotic responses.
Verma recounted his own
lab’s adaptation of adenovirus for use as a gene vector, with the deletion
of the E1a, E1b, and E4 adenoviral genes to blunt its immunogenicity and the
summoning of cytotoxic T cell lymphocytes. The ease of disarming these replication
components and of growing billions of virus particles quickly, as well as adenovirus
infectivity of both dividing and nondividing cells, he said, make it an "attractive"
vector.
University of California
at San Francisco (UCSF) surgical oncologist Robert Warren offered observations
from a trial involving adenovirally packaged p53 delivered via the intrahepatic
artery to the liver of colorectal cancer patients with hepatocellular metastases.
Postinfusion transaminase elevations invariably came down and were never dose
limiting; hypotension, he said, was the dose-limiting toxicity, with liver toxicity
"significantly less than expected." Commenting on questions later
related to the possibility that high doses could mobilize proinflammatory cytokines
and lead to intravascular coagulation, Warren said that duration of exposure
to the vector in his trial may have been too short to observe adverse cytokine
events. "We would expect adenovirus induction of cytokines in the liver,"
he said.
Margaret Rick, hematology
chief in the NIH Clinical Center pathology department, noted that acute hepatic
failure is among possible triggers of DIC. She suggested that patients be screened
for hepatic vulnerabilities to tissue factor upregulation due to infection-
or cytokine-induced endothelial cell damage.
RAC member Estuardo Aguilar-Cordova,
of the Baylor College of Medicine in Houston, suggested that dose-related adenoviral
toxicity may not be linear. "Perhaps there is a threshold effect at a certain
point where only a slight increase in dose results in a great increase in toxicity,"
he said, noting that different species exhibit different levels of inflammatory
response to the equivalent dose and, to make matters more complicated, titer
and dose specifications are not standardized. "It’s not clear we are
all even talking in the same language," he commented, a lament later answered
by Savio Woo, president of the American Society for Gene Therapy, who offered
his group’s services in developing standards for vector quantification.
Phase 1 adenoviral vector–gene
therapy studies have been ongoing at the University of Pennsylvania for the
past five years and have involved 95 patients, 18 of whom participated in the
OTC study. Prior to his detailed account of that trial, Wilson summarized findings
among the 77 other gene therapy patients enrolled in trials addressing cystic
fibrosis and various types of malignancy. "In general," he said, "toxicities
seem to be dose-dependent, time-limited, and confined to the target site."
However, he added, there is a suggestion of "broader cytokine release"
in the presence of fever.
Ron Crystal, chief of
pulmonary and critical care medicine at New York’s Cornell Medical Center,
summarized safety data from gene therapy studies involving E1/E3-deleted adenoviral
vectors of three different transgenes. Among 90 patients with cystic fibrosis,
metastatic colon cancer, or coronary or peripheral vascular conditions that
would benefit from angiogenesis, there have been more than 140 gene administrations,
more than 44,000 follow-up days, and 13 deaths–all related to the patients’
disease and unrelated to therapy dosage. One serious adverse event in a cystic
fibrosis patient was linked to bronchoscopic delivery and has not recurred since
a switch to aerosol spray, he said. Adverse pulmonary events were found to be
dose related in animal studies conducted by the Genzyme Corporation (Cambridge,
Mass.).
The
OTC Trial
The prelude, conduct,
and aftermath of the OTC trial were presented by Batshaw, Raper, and Wilson.
Using the sparse fur mouse as a model, they delivered what would have been a
fatal ammonia dose to animals pretreated with the adenoviral OTC gene vector.
The ensuing rapid drops in glutamine and ammonia concentrations matched the
speed the investigators sought to prevent the irreversible brain damage sustained
by children who manage to survive coma longer than 72 hours. The adenoviral
vector evolved from an E1-deleted to an E1-deleted/E2-mutated and, finally,
to an E1/E4-deleted construct.
Although newborns with
full-blown OTCD were the population for whom the gene therapy was ultimately
targeted, it was decided that the study cohort for this first experiment to
determine safety would be stable adults with partial disease who could give
informed consent.
The investigators submitted
their protocol application to the RAC in March 1994, when the RAC still had
approval authority, along with the FDA, for all gene therapy protocols. In 1995,
the RAC approved the protocol contingent on what members concluded would be
a safer route of administration: intravenous, rather than intrahepatic. The
FDA, however, later opted for intrahepatic delivery, in part to lessen the possibility
of unintended delivery of the transgene to the gonads. The RAC was never informed
of the protocol modification.
"We recognize that
we probably should have gone back to the RAC to discuss this," Batshaw
said, "but RAC’s responsibilities were changing. . . . We apologize."
Wilson issued the same apology during his presentation later that day.
FDA approved the protocol—with
the intrahepatic artery route—in 1996; the first patient was dosed in April
1997; and Jesse Gelsinger, the last patient, was dosed in September 1999.
OTCD
in General and in the Case of Jesse Gelsinger
Ornithine
transcarbamylase deficiency (OTCD) is an inborn error of metabolism
in which the second enzyme in the urea cycle is missing; it affects
one in 40,000 to 80,000 children. The inability to excrete urea can
precipitate an acute rise in ammonia concentrations, brain damage, coma,
and death. Neonatal mortality within the first month is 50 percent,
and 50 percent of early survivors die within the first five years. Without
a liver transplant, 75 percent of survivors will sustain severe neurological
dysfunction.
Patients with partial OTCD
have some residual enzyme activity and can be managed on a strict low-protein
diet and the "alternative pathway" regimen (intravenous sodium
benzoate, sodium acetate, and arginine hydrochloride), co-developed
by Mark Batshaw, principle investigator in the UPenn study. They are
always at risk of coma, however, and the therapy, says Batshaw, is "incomplete
at best." Jesse Gelsinger’s partial OTCD was diagnosed at
33 months, when he presented lethargic, incoherent, and with elevated
ammonia and glutamine concentrations. He was hospitalized at age 10
and again in December 1998. In June 1999, he met screening criteria
for the UPenn trial, but his ammonia concentration the day before actual
dosing three months later exceeded the cutoff for entry eligibility.
He was placed on the alternative pathway regimen, hydrated, and the
next day, September 13, dosed as per protocol. He died on September
17. Though the relationship of his death to his liver function at dosing
had not been established, co-investigator Steve Raper asserted that
"We agree that future inclusion criteria" should address standards
of patient status directly before dosing.

|
All told, four men and
14 women participated in the trial. High fever post-infusion was frequent, as
were backache and nausea. Drops in platelet counts and phosphates were dose
related and increased over the course of the cohorts (the protocol called for
six cohorts, with three patients in each—the first two women and the last
a man—to receive doses escalating in half-log increments beginning with
2 times 99 particles/kg and ending with 6 times
1011). Similarly, transaminase elevations appeared to be dose related, but not
consistently.
An odd and surprising
finding related to antibody response to the vector: adenovirus-naive patients
developed an expected lymphoproliferative response (LPR), but those who had
antibodies to begin with experienced a "transient LPR loss," a phenomenon
some panelists viewed as a safety concern in the context of inadvertent exposure
to adenovirus infection during LPR downtime. This loss of T cell ability to
respond to adenovirus, Wilson said later that day, was not seen in any other
clinical or animal trials.
In general, the team was
concerned about platelet lowering and its relation to vector dose. In collaboration
with FDA, the team began DIC monitoring with the second cohort, tracking platelet
counts and fibrin split products before, during, and after infusion and keeping
an eye out for the presence of vector in the systemic circulation.
But it was not until the
fourth cohort that there were recurring problems that the investigators were
required by protocol to report to FDA before proceeding with subsequent dosing.
These involved marked elevations in liver function assays, two of which were
reported in a timely manner and two of which were not. Raper acknowledged these
lapses: "We should have called FDA before dosing patient 14, and
we should have made another call before proceeding to the next dose level,"
he said.
Other irregularities mentioned
by FDA officials during the meeting but not addressed publicly by the investigators
included the investigators’ failure to get FDA permission to have a man
(Jesse Gelsinger) replace a woman as the second patient in his cohort and that
information in the consent form submitted to FDA—that primates had died
on high doses in preclinical studies—was removed from the final consent
document.
When Raper turned to the
specifics of Jesse Gelsinger’s clinical course, he did not address a question
raised during the meeting: whether the investigators should have proceeded to
infuse Gelsinger in the face of abnormal liver function tests that required
alternative pathway therapy prior to dosing. He later implied that patient status
before infusion should be rethought.
Gelsinger’s
Course
Gelsinger’s status
eight hours postinfusion was not unlike that of other study participants. Raper
said: he had a fever, normal liver function tests, and no evidence of DIC; he
was given intravenous potassium phosphate for low phosphate concentrations.
The morning after, however, nurses noticed an altered mental state; his ammonia
concentration had risen, and he was jaundiced and tachycardic. A coagulation
workup showed increased prothrombin time and fibrin split products and decreased
platelets.
He became "progressively
obtunded" and by the second evening he was comatose. Chest X-ray showed
infiltrates suggestive of ARDS. Raper described a series of developments in
Gelsinger and actions taken by medical teams to offset or reverse what eventually
became what he called a "desperate lung situation." These measures
did not save the patient.
Commenting generally on
Gelsinger’s clinical course and the efforts to save his life, UCSF’s
Warren later observed that "each intervention seemed logical and appropriate"
but did not prevail against the "cascade of irreversible events."
With the Gelsinger family
permission, Raper said, a postmortem examination was performed. There was little
vector-induced hepatitis and no significant signs of DIC. Jesse Gelsinger died
of intractable ARDS, with anoxia evident in the liver, kidney, brain, and spleen.
The team speculated that ARDS was secondary to "secondary inflammatory
response syndrome," referred to by Raper as "immune revolt."
Bone marrow yielded "perhaps
the most unexpected findings: an absence of erythroid precursors and mature
granulocytes, suggesting acute insult."
The team speculated that
the anemia could be an idiosyncratic reaction to the medications or a sign of
human parvovirus infection. One RAC consultant noted during discussions later
that the one disease associated with such acute and striking bone marrow aplasia
is parvovirus infection.
Questions
"We in no way expected
to see what we saw in Jesse Gelsinger. Our animal studies never demonstrated
these pulmonary events," said Wilson, who presented a chronology of the
team’s vector manipulations and animal studies—including mice, newborn
and adult rhesus monkeys, and baboons—and ruminated on the cytokine findings
in Gelsinger’s case and the questions remaining to be answered.
Test animals, he said,
had demonstrated self-limited, dose-dependent hepatitis, a transient decline
in platelets, and transient transaminase elevations, with an apparently biphasic
dose-toxicity relationship. Dose-limiting toxicities were liver damage and DIC
at significantly higher doses, he said, than that received by Gelsinger. UCSF’s
Warren commented: "We have not seen the pulmonary dysfunction in our 60
patients that you saw with Jesse Gelsinger."
Wilson elaborated on Gelsinger’s
immune response to the vector, as well as vector biodistribution on autopsy.
At the higher vector doses received by patients in the last two study cohorts,
there were rapid, dramatic cytokine increases, specifically of interleukin-6
(IL-6) and IL-10. Recovery followed in all cases but Gelsinger’s, whose
IL-6 trajectory never returned to base line. "Maybe we are activating some
aspect of the immune system," Wilson said, suggesting that some "inciting
event of acute cytokine release" from macrophages and monocytes had occurred.
"What was different about this patient?" he asked—and listed
hemodialysis, intubation, and external ventilation among the atypical procedures
Gelsinger had undergone.
The investigators used
PCR to track the vector after hepatic artery infusion. The highest DNA concentration
was found in the liver—first in the macrophages (Kupffer cells) and then
the hepatocytes—with significant amounts also appearing in the spleen,
lymph node, and bone marrow. Biodistribution, Wilson remarked, "was not
as hepatospecific as I had hoped." RAC co-chair Verma later noted that
animal models are generally not good enough to pinpoint biodistribution. He
cited the fact that rhesus monkeys and humans do not have the same CAR distribution.
After the death, the team
studied the specific vector lot Gelsinger had received, as well as the equivalent
of the preceding lot, and tested them at the same doses in rhesus monkeys. "Clinically,
the animals did fine," Wilson said.
Among issues to be investigated,
he said, are what role, if any, Gelsinger’s underlying condition and medications
played in his outcome; whether he had a genetic predisposition to such an outcome;
why the vector distributed beyond the liver and whether this affected outcome;
and what stimulated cytokine release and, again, whether this affected outcome.
"We don’t know the roles of IL-6 and IL-10," he emphasized.
Asked what he would have
done differently, Wilson replied, "Including not having done this at all,
the trial could have been designed differently [with respect to] the half-log
increments. The increments should be smaller." He noted that the dose-toxicity
relationship appeared to be "elbow shaped" and that at the half-log
increment the difference in dosage between the later cohorts is significantly
greater than that between the earlier ones and "may be breaching that elbow."
A RAC member agreed that there appeared to be a "narrow window between
early and severe toxicity, requiring meticulous measures."
FDA’s investigation
into the conduct of the UPenn trial was ongoing at Catalyst press time.

|
Gene
Therapy Oversight
 |
Overseers Answer the
Press (left to right): Amy
Patterson, director,
NIH Office of Biotechnology Activities; Lana
Skirboll, director, Office of NIH Science Policy;
Phil Noguchi, director, FDA Division of Cellular and Gene Therapies;
and Kathryn Zoon, director, FDA Center for Biologics Evaluation
and Research, respond to questions during a news briefing after
the first day of the RAC meeting. Nearly all questions centered
on FDA's oversight role in the OTC study, protocol violations,
and FDA's steps to uncover, punish, and prevent irregularities
in gene therapy clinical trials.
|
The
rules and roles of federal agencies involved in overseeing gene therapy
experiments are undergoing review and may be revised in the wake of Jesse
Gelsinger’s death. Specifically, the role of the NIH Recombinant
DNA Advisory Committee (RAC) is being revisited, and proposed amendments
to the NIH
Guidelines for Research Involving Recombinant DNA Molecules
(NIH Guidelines) have been published. The harmony—or
lack of it—between NIH and FDA adverse event reporting requirements
in the conduct of clinical trials is also being scrutinized.
Revisiting
the RAC. Before vacating the office of NIH director, Harold
Varmus announced the formation of a subcommittee of the director’s
advisory group to recommend further actions NIH might take to minimize
adverse events in gene therapy trials. Although the group’s charge
also places the role of the RAC back on the table, Varmus stands by his
actions in 1995 to recast the RAC from a quasi-regulatory body with approval
authority over every gene therapy application.to a public policy forum
on novel methods in gene therapy clinical trials and thorny issues related
to gene therapy (see Harold Varmus interview,
this issue).
NIH
Guidelines. NIH clarified the definition of adverse events
and investigators’ reporting obligations in a proposed action to
amend the NIH Guidelines, published in the Federal Register
November 22, 1999.
The proposal reaffirms that
investigators must report serious adverse events immediately to NIH, so
NIH may rapidly notify the RAC and others involved in gene transfer studies.
"Immediately" is defined as no later than 15 days from the event.
A "serious adverse event" is defined as any "expected or
unexpected adverse event, related or unrelated to the intervention, occurring
at any dose" that results in death, a life-threatening event, hospital
admission or prolonged stay, or disability.
It also rejects recent claims
by some gene therapy investigators and sponsors that human gene transfer
protocols and serious adverse event reports are trade secrets. Informed
consent documents would reflect the necessarily public nature of RAC discussions
of adverse events.
The NIH Guidelines
require the principal investigator to report serious adverse events to
local review bodies and the FDA as well as to NIH and the federal Office
of Protection from Research Risks. FDA reporting requirements require
the study sponsor (who has presumably been informed by the investigator)
to immediately report serious and unexpected adverse events
to FDA. NIH proceedings are public; FDA proceedings are often closed.
During the RAC proceedings,
industry representatives accepted the need for immediate reporting only
of "related and unexpected" serious adverse events, and some
RAC members voiced skepticism that they could deal meaningfully with reports
of all adverse events.

–F.P.
|
Return to Table of Contents